In November 2022, Abdullah Darwich, a nonverbal autistic 19-year-old left his home in Mississauga, Ont. He made his way to a pile of leaves, which he began playing in, dressed only in his underwear. A worried neighbour made a phone call to the police. Despite Darwich being registered to the Peel Police Vulnerable Persons Registry, Darwich’s father arrived soon after to find his son bleeding, terrified and surrounded by police.
When a review was conducted into the incident, the first responding officer explained that he thought Darwich was experiencing excited delirium. As a result of this assessment, the officer thought it necessary to taser Darwich, restrain him and call for backup. The review found no reasonable grounds for misconduct.
How did this happen? At first glance, it may seem unimaginable that Darwich, an unarmed autistic teenager playing in leaves, was perceived as a threat. However, a closer look at the diagnosis of excited delirium and how it shapes police conduct reveals why this incident is not only unsurprising, but predictable.
Table of Contents
Excited delirium
The diagnosis of excited delirium — a condition in which individuals become agitated, are impervious to pain and display unnatural strength — has come under increasing fire recently. Those questioning its validity, and the conflicts of interest surrounding its promotion, include the American Psychiatric Association, the American Medical Association, and Physicians for Human Rights.
In the United Kingdom, police are now barred from using the term to explain deaths taking place in the context of restraint. California and Colorado recently banned the use of the term in coroner’s reports, and Colorado also removed it from police training. Coroners in four Canadian provinces say they no longer accept it as a cause of death.
These are all moves in the right direction. However, this troubling term remains in circulation in Canada, the United States and elsewhere, particularly in law enforcement, emergency medicine and on coroner’s reports. And it can have a dangerous influence on what police officers see and do.
‘An agitated and delirious state’
Excited delirium has been described as “an agitated and delirious state” that often involves sweating, rapid breathing, pain tolerance, superhuman strength and “a failure to respond to police presence.” Many police officers are exposed to this diagnosis in training, and instructed to look for signs of excited delirium when encountering members of the public who may seem distressed. The appropriate response, they are taught, is often “overwhelming force.”
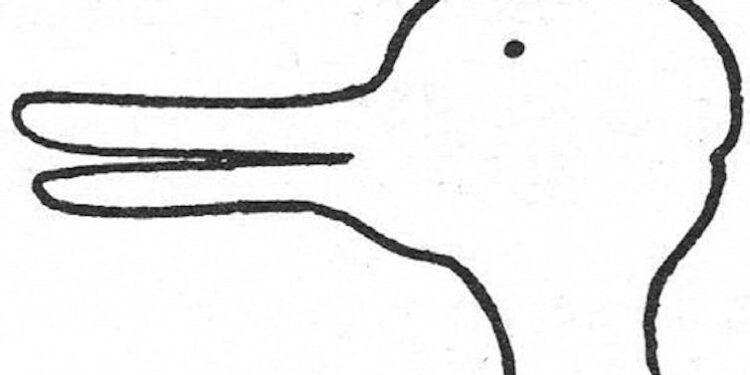
Beyond merely educating police officers about the key symptoms of excited delirium, this training also impacts what police are likely to see when on the job. Our perceptions are inevitably shaped by what we believe and expect. Philosophers of science call this theory-ladenness. Whether you see a duck or a rabbit in the image below depends on what you expect to see:

(Ludwig Wittgenstein ‘Philosophical Investigations’ p. 194)
Theory-ladenness shows up everywhere. What a meteorologist sees when they look at a weather map is different than what a lay person sees. An ultrasound technician can identify much more on an ultrasound than I’m able to. A kiss your toddler is giving to their friend seems charming, until you realize it’s actually a bite. Similarly, the theory of excited delirium shapes what police perceive.
Rather than seeing a scared teenager who communicates in a different way than others, an officer saw Darwich as a threat. He explained in an interview that when Darwich didn’t seem to be experiencing pain and stress from being stunned with a Taser, he thought it must be a case of excited delirium.
Police training
Research shows Black, Indigenous and other racialized people are more likely to experience over-policing than those who are white. The description of excited delirium offered in police training is of someone who is superhuman, insensitive, feral and must be stopped at all costs. This image aligns with historical depictions of Black, Indigenous and other non-white bodies thought to be less sensitive to pain and more emotional than white ones. These stereotypes still circulate today, with more than half of American medical students and residents in a 2016 survey endorsing the statement “black people’s skin is thicker than white people’s skin.”
In training manuals about excited delirium, pictures of people of colour said to be experiencing excited delirium are often used, many of them nearly naked and in vulnerable positions, reinforcing these biases. A preponderance of data indicates that racialized people are more likely than white people to be labeled with excited delirium and to experience force and restraint at the hands of police.
Taking this into account, the incident with Darwich feels less surprising. If officers are taught to look for excited delirium, and see it in some people more than others, there will inevitably be false positives.
Unfortunately, Darwich’s case was not unusual. The same month, another nonverbal autistic teenager was tased by police in Québec. The month before, a man experiencing a seizure was tased by police in Hamilton, Ont. None of these individuals were white.
Excited delirium under fire
Fortunately, Darwich recovered from his injuries, but many others have not. Eric Parsa, a 16-year-old autistic teenager, was killed by police in Louisiana in 2020 after being pinned to the ground and sat on for more than nine minutes. In this case, excited delirium was not only used to justify force, but to explain Parsa’s death.
In Parsa’s case, and many others (Daniel Prude, Clive Mensah, Abdirahman Abdi), excited delirium is used as an explanation of death on a coroner’s report, distracting attention away from restraint and force (chokeholds, hogties, tasers), which is always also present. The pseudo-diagnosis is a slippery one, sometimes linked to mental illness, other times drug use, and in other instances, bad genes, a bad heart or bad blood.
Recently, however, the coroner’s office agreed to remove the term excited delirium from Parsa’s death report, noting that other factors were enough to explain the death. Parsa’s father said the removal of this term has “truly helped in our healing process.”
This, and other strides being made towards recognizing the damage this diagnosis can cause, give us reason to be hopeful. Four provinces in Canada have removed the term from use; others should follow suit. Law enforcement and those working in emergency medicine can work towards eliminating this term from both training and circulation.
However, as excited delirium falls out of favour, we must be wary of new language that might slip in and take its place. Other candidates are already emerging, including “acute behavioural disturbance,” “hyperactive delirium with severe agitation” and “autonomic hyperarousal state.” This means we need to fundamentally rethink how we respond to those experiencing distress, not merely the language we use to describe them.
![]()
Phoebe Friesen does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.