
Personalized medicine describes a treatment tailored to one or a few individuals who have potentially deadly health conditions, such as cancer that no longer responds to chemotherapy, or an infection resistant to multiple antibiotics.
Although personalized medicine is promising, it is labour-intensive and expensive, and the pathways for its regulatory approval and reimbursement are complicated, since the small number of patients who qualify limits the design of clinical trials.
Here we use recent examples of chimeric antigen receptor (CAR) T-cell therapy for relapsed cancers, and bacteriophage (phage) therapy for antibiotic-resistant bacterial infections, to show how Canadians could benefit from these personalized solutions.
Challenges that need to be overcome include ensuring equitable access, and deciding who should cover the cost of these important medical advances.
Table of Contents
CAR T-cell therapy for cancer that relapses after chemo
CAR T-cell therapy was first approved in 2017. In CAR T-cell therapy, the patient’s own white blood cells are harvested and modified in a lab to better identify and destroy the specific tumour. The modified cells are then placed back into the patient, where they attack the cancer.
CAR T-cell therapy has great potential for treating certain types of advanced leukemia or lymphoma. Many patients reach remission after the treatment, and some even have a long-term cure.
For example, the first CAR T-cell therapy led to over 80 per cent remission at three months post treatment and 62 per cent remission after two years. Emily Whitehead, the first pediatric patient to receive CAR T-cells, is still cancer-free 12 years after her treatment in 2012, even though her life expectancy before the therapy was only a few weeks.
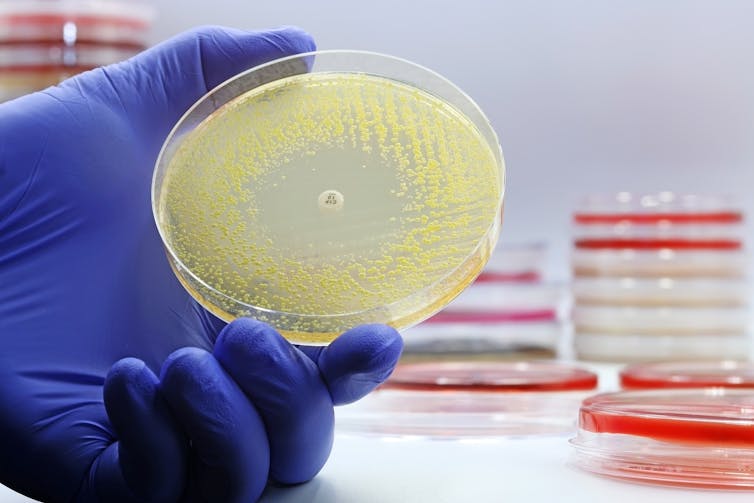
Bacteriophage therapy for antibiotic-resistant superbugs
(Shutterstock)
Another patient-specific treatment uses phages: viruses that kill bacteria but are harmless to people and animals. They were discovered over a century ago by a French-Canadian microbiologist, Félix d’Hérelle and used to treat infections prior to the discovery of antibiotics.
As global rates of antibiotic resistance rise, people are turning back to phages to treat otherwise untreatable “superbug” infections.
Phages are picky eaters, so it’s necessary to carefully match the bacteria causing the infection with phages that recognize them as prey. Multiple types of phages are typically combined in a “cocktail,” to reduce the chances of the bacterium evading recognition by the phages.
The first modern Canadian trial of phage therapy for a drug-resistant urinary tract infection (UTI) in 2023 was a success. The patient had already lost a kidney to her infection, which could not be resolved with antibiotics alone.
In another recent example, a patient with a challenging infection of her artificial hip was successfully treated using phage therapy.
Manufacturing, approval and reimbursement challenges
Personalized medicine is expensive. This is partly due to the fact that manufacturing personalized therapies is highly complex and the customization required limits the ability to achieve economies of scale that could lower costs. Methods for manufacturing could be standardized to some extent, but there will be features unique to each patient.
For example, although phages are abundant in nature and easily found, matching the right ones to an individual patient’s superbug takes significant time and effort. There are few manufacturers that can prepare clinical-grade phage cocktails on short notice if standard antibiotic treatments fail.
In the case of CAR T-cell therapy, the patient’s own cells must be harvested and modified to target their specific tumour. This process requires rigorous quality control, advanced training and equipment, and a single infusion can cost over US$350,000. Pre- and post-treatment expenses may bring the actual price closer to US$1 million. This hefty price tag places a heavy burden on the health-care system and presents a major barrier to access.

(Shutterstock)
To decrease costs associated with third-party manufacturing abroad, Canadian researchers have begun testing new methods of manufacturing CAR T-cell therapies directly in Canadian academic institutions.
Health Canada’s standard drug regulatory approach was designed for approval of one therapeutic for many patients, using evidence from large clinical trials. Personalized medicine requires a new approach that allows for approval of individualized treatments for a much smaller group, or even a single person.
Therapies with small patient population sizes may be evaluated under Health Canada’s new Notice of Compliance with Conditions (NOC/c) pathway, which allows promising treatments to have conditional market access. Full approval at a later date is contingent on the collection of more clinical evidence.
This pathway speeds up the approval process so Canadians can more quickly get access to treatments for life-threatening or debilitating illnesses. Further changes to regulatory processes may be required to accommodate an increasing number of personalized medicines.
Alternatively, Canada could follow the lead of Belgium, who took the approach of pre-approving a large set of individual phages, that could then be combined in unique ways for each patient without further regulatory steps. They recently published data for the first 100 cases, reporting high rates of success.
The small sample sizes and lack of standardization of personalized medicine can make it harder to evaluate its health economic impacts, which governments traditionally rely on for approval and reimbursement decisions. Canada has started to supplement with real-world data/evidence from clinical databases in cases where large trials are not feasible. Such information includes patient or health delivery data that is already routinely collected from a variety of sources, including electronic health records or digital health technologies.
Strategies to boost access
However, challenges remain in how we gather and integrate information across our diverse provincial health-care systems. The Canadian government recently invested $20 million to improve the collection and use of real-world evidence for regulatory decision making as part of a strategy to boost access to drugs for rare diseases, another case where patient numbers are low but disease impact can be high.
New methods to evaluate the cost-effectiveness of personalized medicine will also be important. Such evaluations measure the prevalence of disease, accuracy of diagnostic tests, treatment effectiveness, probability of complications, availability of better treatments, and quality-adjusted life-years to justify the price of a treatment. Having a clearer idea of the cost-savings ratio of personalized medicine will help to justify the use of limited health-care resources.
Implementing an outcomes-based reimbursement model could also address cost, reimbursement and access concerns. Here, payments would only be made if the patient responds to treatment by a certain time point. Patient assistance programs will also be crucial to offset some of the costs. These are sometimes offered by pharmaceutical manufacturers to provide prescription drugs to eligible patients at low or no cost.
The field of personalized medicine will continue to grow, with more innovations emerging for an increasing number of indications. Ensuring timely and affordable access to these therapies in the face of their high costs and smaller patient populations will be of utmost importance. Success with require collaboration between pharmaceutical companies, government agencies, insurance companies and health-care institutions.
![]()
Lori L. Burrows receives research funding from the Canadian Institutes of Health Research, the Natural Sciences and Engineering Research Council of Canada, and holds the Canada Research Chair in Microbe-Surface Interactions.
Elizabeth C. Li does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
























