
Despite researchers’ efforts to understand SARS-CoV-2, the virus continues to hold many secrets. As much as we’ve tried to shoehorn it into our thinking about how respiratory viruses work, it will simply not comply.
Some thought the virus would settle into a strictly seasonal pattern. It hasn’t.
Some thought we could we move to a single annual vaccine every autumn. That was upended by having multiple waves of infection each year, that seem to occur in the late summer.
Some variants we thought would be terrible turned out to be mild, while others have turned out to be very problematic.
Table of Contents
Surprising study results
Now we have a new puzzle.
Through the first couple of years of the pandemic before the emergence of the Omicron variant, it was believed the combination of vaccination and prior infection — which is called hybrid immunity — provided the highest level of protection against future infections.
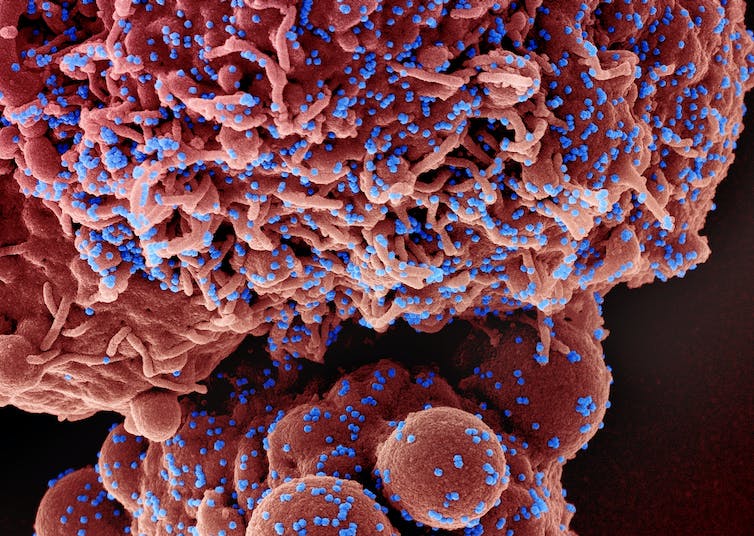
NIAID, CC BY
Our research group has been studying vaccinated older adults in long-term care and retirement homes throughout the pandemic, and our recent findings have jolted us.
We found that those who had battled the BA.1-2 variant of Omicron in early 2022 had a 30-fold higher risk of contracting the BA.5 variant later in the year. That was exactly the opposite of what we, or anyone, would have predicted.
This new knowledge is critically important, not just to other older adults, but to all of us.
Does this surprising twist apply to the broader population? Possibly, but until we know how infections work to increase susceptibility to reinfection, we can’t know if this susceptibility is specific to older adults. Does it apply to other variants, including the newest ones in circulation? That’s unclear.
What the findings do tell us is that older adults who have had a previous COVID-19 infection shouldn’t rely on that to protect them against reinfection this fall. To protect against severe illness, keeping booster shots up to date is recommended.
We can’t let our guard down
We were able to make this discovery because our study participants in long-term care and retirement homes are part of the most frequently tested, highly vaccinated and closely observed group in the entire population.
The end of frequent PCR testing and documentation of infection for those who are sick (after all, we researchers don’t know if you tested positive on a rapid test) left us without much data about COVID infections and reinfections in the broader population, so these seniors are helping us see things we’d otherwise have missed.
Through them, we’ve realized the virus has evolved in a way that means one infection doesn’t necessarily guarantee immunity from another.
Though we still have so much to learn about many aspects of COVID-19 — including its lingering health effects and the mechanics of its endless mutations — we do know enough to say one thing: we can’t let our guard down.
Read more:
Long COVID: For the 1 in 10 patients who become long-haulers, COVID-19 has lasting effects
Among other conclusions, we know that while vaccines mitigate the worst consequences of subsequent COVID infections, the virus is still developing new ways to elude our immune systems.
Protecting ourselves and our communities
So, do we still need masks and boosters? Yes. However tiresome they have become, they’re still crucial. This is especially true for our most vulnerable, including older adults, people with chronic conditions or who are immune compromised and those who work with them.

(Shutterstock)
We know the protective value of multiple COVID vaccines does not accumulate like money in a bank account. It’s the recency of our boosters that will determine our degree of protection.
Though imperfect, timely boosters are still our best shields. It’s time to think of them less like our childhood vaccines, where we expect to be protected for long periods of time, and more like annual flu vaccines where we need to be vaccinated for the strain that is circulating and can only expect that protection to reduce symptomatic infection, last a few months but — importantly — help keep us out of hospital.
We need to remain vigilant and to continue to keep our vaccines up to date, to protect against COVID infections and their threat of debilitating long-term effects and even death.
Protecting ourselves and our communities
Our participants have been great partners in our work. As a group, and are willing to participate in this research because they are interested in helping others. They helped us discover that hybrid immunity does not always protect older adults from future COVID-19 infection, suggesting that some assumptions about COVID-19 infection risk may need to be revisited, and that we need to study how different variants evade the immune system.
These research partners deserve the thanks of the community for contributing to this important lesson. We can all honour them by heeding that lesson and taking precautions against spreading COVID-19 this fall, including wearing masks and getting a booster shot.
![]()
Dawn ME Bowdish received funding from the COVID-19 Immunity Task Force/Public Health Agency to perform the research described herein. She is a member of the Board of Directors of the Lung Health Foundation.
Andrew Costa received funding from the COVID-19 Immunity Task Force/Public Health Agency to perform the research described herein.























