
APIMerah/Shutterstock
I’ll often lie awake until three or four in the morning, before drifting off for just a few hours. Then comes the dreaded alarm clock. My mind and body are exhausted all the time – there’s always this knot of anxiety in my chest, doing away with any hope of a good night’s sleep.
Simon* is a NHS mental health nurse who, like millions of people in the UK, suffers from insomnia: a sustained difficulty in initiating and maintaining sleep. His job is to support the recovery of people with severe mental illness, but his own sleep problems have had a profoundly negative impact on his mental health.
Most of us experience a bad night’s sleep from time to time, but can usually get back on track within a night or two. People suffering from insomnia, by contrast, have sleep problems that last for months or years at a time, taking a major toll on their health and wellbeing.
Around a third of people will experience insomnia at some point in their life, with women and older people more often affected. Nearly 40% of sufferers fail to recover within five years. People with insomnia have an increased risk of diabetes, high blood pressure and cardiovascular disease. Insomnia is also a major risk factor for mental illness, and often co-occurs with mood disorders such as depression and anxiety.
Across the world, we’re seeing unprecedented levels of mental illness at all ages, from children to the very old – with huge costs to families, communities and economies. In this series, we investigate what’s causing this crisis, and report on the latest research to improve people’s mental health at all stages of life.
Many different life events can increase your chances of sustained sleep deprivation. Both the financial burden and confinement arising from the COVID-19 pandemic were associated with greater risk of insomnia, which is in turn likely to have led to a rise in mental health problems.
And yet, very little is known about why and how a prolonged absence of sleep gives rise to mental illness. Our team at the University of York has pioneered research into whether sleep deprivation disrupts the brain’s ability to suppress intrusive memories and distressing thoughts – classic symptoms of psychiatric disturbance.
It has also led us to ask whether it might one day be possible to treat mental illness while patients are sleeping – for example, by using sounds to normalise irregular patterns of brain activity during rapid eye movement (REM) sleep.
Table of Contents
Why are some people so badly affected?
They put their hand over my face so I couldn’t breathe. Now I can’t wear anything that covers my mouth or nose for fear of reliving [that experience]. Mask wearing was a big problem for me during the pandemic – and it was always worse when I slept badly. Just the sight of other people wearing masks could bring it all back.
Helen* is a domestic abuse survivor who suffers from post-traumatic stress disorder (PTSD), a debilitating condition characterised by flashbacks, nightmares and severe anxiety. She told us her symptoms would always get worse after a bad night’s sleep – a pattern reported by other PTSD sufferers we spoke to.

Randoms/Shutterstock
We can all sometimes encounter intrusive and unwanted thoughts, usually in response to reminders – for example, seeing a former partner and being reminded of an unpleasant breakup. While unsettling, these thoughts are infrequent, short-lived and, usually, quickly forgotten. This is in stark contrast to the highly lucid, distressing thoughts experienced by people with PTSD. Sufferers often engage in avoidant behaviour, such as not leaving home to reduce the likelihood of having to confront reminders of their trauma.
However, the symptoms of PTSD can also partly be explained by a breakdown of the brain mechanisms we rely on to push such intrusive thoughts out of conscious awareness. Because intrusive thoughts arise from unpleasant memories, another way people ward them off is by suppressing the offending content from their memory. But PTSD sufferers often exhibit a deficit in their ability to engage in this process of memory suppression, resulting in persistent unwanted patterns of thinking.

This article is part of Conversation Insights
The Insights team generates long-form journalism derived from interdisciplinary research. The team is working with academics from different backgrounds who have been engaged in projects aimed at tackling societal and scientific challenges.
And what if lack of sleep reduces our ability to suppress unwanted thoughts and memories? This could lead to a downward spiral of more persistent and frightening intrusive thoughts, severe anxiety, and chronic sleeplessness – culminating in psychiatric disturbance.
Although a wealth of research has shown that sleep deprivation leads to psychological instability, our study was the first study to examine how an inability to control intrusive thoughts might underpin this relationship. For this reason, we worked with young adults without a diagnosed mental health disorder, allowing us to determine how even healthy brain processes go awry when people do not get enough sleep.
How sleep deprivation affects our brain
Our group of young adults (aged 18–25) were asked to memorise face-image pairs, comprising a male or female face with a neutral expression next to a unique scene. They would memorise each pair over and over again, so that any face presented in isolation would serve as a powerful reminder of the scene it was paired with – in the same way a reminder of an unpleasant event in the real world can trigger a distressing thought.
The face-scene learning took place late in the evening – after which half the participants went to sleep in our laboratory, and the other half stayed awake for the entire night – watching movies, playing games and going for short walks outside. They could eat and drink, but psychological stimulants such as caffeine were strictly prohibited. We would wake anyone in this group who nodded off.
Next morning, all participants were shown the faces only, in random order, with the following instructions. If the face was inside a green frame, the participant should allow the associated scene to come into their mind. A red frame meant they should engage in memory suppression to block out the scene – in the same way we sometimes purge unwanted thoughts from our conscious experience.
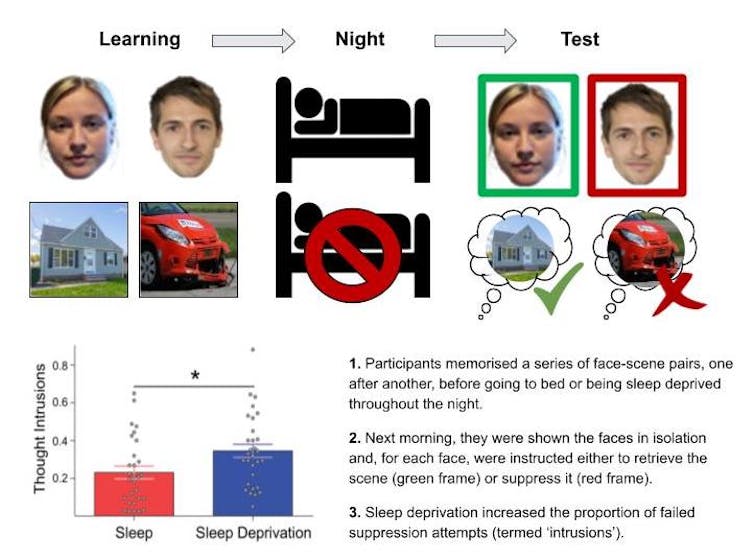
Scott Cairney/University of York, CC BY-NC-SA
Our sleep-deprived participants reported having more “intrusions” (failed memory suppression attempts) than those who had slept normally. And only well-rested participants got better at suppressing the unwanted memories over time. This suggests that sleeplessness does long-term harm to our ability to suppress intrusive memories and, hence, unwanted thoughts.
What’s going wrong inside a sleep-deprived person’s brain? To address this question, we repeated our study, but this time with participants undergoing functional magnetic resonance imaging (fMRI) – a powerful neuroimaging technique that allows us to determine which brain regions are engaged during particular cognitive operations (in this case, keeping intrusive memories at bay).
Memory suppression relies on a brain region known as the right dorsolateral prefrontal cortex (rDLPFC). When a reminder triggers retrieval of an unwanted memory, the rDLPFC inhibits activity in the brain’s memory processing centre, the hippocampus, to push that memory out of the person’s mind.
Our fMRI study showed that, when participants were attempting to suppress unwanted memories, activity in rDLPFC was reduced after a night of sleep deprivation relative to a night of restful sleep. Moreover, activity in the hippocampus was stronger after sleep deprivation than restful sleep, suggesting that a breakdown of control by rDLPFC had allowed unsolicited memory operations to emerge with impunity, opening the door to intrusive patterns of thinking.
Can better sleep improve our mental health?
REM sleep, discovered by Eugene Aserinsky and Nathaniel Kleitman in 1953, is a unique stage of sleep characterised by rapid movement of the eyes and a high propensity for vivid dreaming.
As the brain enters REM sleep, it undergoes dramatic changes that are thought to play an important role in regulating our mental health. For example, levels of the neurotransmitter acetylcholine, which modulates the processing of disturbing memories, are markedly increased in REM sleep relative to other sleep stages, mirroring levels seen in wakefulness. Abnormalities of REM sleep are linked to various psychiatric mood disorders including PTSD, and associated with the intense nightmares experienced following trauma.
Read more:
A short history of insomnia and how we became obsessed with sleep
So, could the brain mechanisms that allow us to control intrusive memories be especially influenced by the amount of REM sleep we obtain over the course of a night? To investigate this, our fMRI study included polysomnography – a sleep monitoring technique that enabled us to identify when participants were in REM sleep, based on both their eye movement and discrete brainwave patterns.
Among our participants who slept, those who had more REM sleep showed stronger engagement of their rDLPFC when suppressing unwanted memories the next morning. This suggests REM sleep may indeed support mental health by restoring the brain systems that help to shield us from unwelcome thoughts.
The emotional intensity of our memories
When we think back to a traumatic or painful life event, we get a sense of the unpleasant feelings, such as sadness or anger, that accompanied the original experience. However, the intensity of these feelings is usually much reduced, allowing us to draw on past events without being consumed by negative emotions.
Suppressing unwanted thoughts has been shown to weaken the memories that lead to them, meaning they are less likely to intrude into our consciousness in the future. This relates not only to the content of the memories (the “what, when and who”) but also their emotional charge – the intensity of the emotions we felt at the time. In other words, memory suppression helps us move on from prior adversity by gradually cleansing our memories of unpleasant experiences, and the negative emotions associated with them.
Conversely, failing to suppress an unwanted memory is likely to cause its emotional charge to linger, meaning that emotional responses to future reminders will remain more intense.

APIMerah/Shutterstock
We tested this by showing our participants scenes that were either emotionally negative (such as a car crash) or neutral (such as a forest). In the morning, after completing the memory retrieval and suppression task (with green and red-framed faces), participants were then asked to give intensity ratings for the negative and neutral scenes again.
Our findings were clear – and corroborated by further tests using an objective index of emotional arousal, skin conductance responses. Among participants who had slept, emotional responses to the suppressed negative scenes became less intense over time. But among the sleep-deprived, emotional ratings for negative scenes remained elevated, regardless of whether the scenes were suppressed or not. This suggests that a breakdown of memory suppression mechanisms after sleep loss prevented participants from being able to “deal with” these negative emotions.
Read more:
Insomnia and mental disorders are linked. But exactly how is still a mystery
In the context of psychiatric mood disorders that co-occur with chronic sleep disturbance, failure to suppress memories of emotionally disturbing events, together with an inability to reduce the unpleasant feelings embedded within those memories, could contribute to a strong tendency of mood-disordered individuals to focus on negative interpretations of the past.
Furthermore, anxiety arising from intrusive memories may also obstruct the sleep that is needed for recovery, leading to a vicious cycle of emotional dysregulation and sleeplessness.
The importance of forgetting
In the film Eternal Sunshine of the Spotless Mind (2004), the main characters have their memories of their turbulent relationship erased. Far from improving their quality of life, this leads to further complications, serving as a cautionary tale.
However, there are situations where aiding the forgetting process may help. For example, people who have experienced traumatic experiences can struggle to cope with unwanted memory intrusions. In these extreme cases, where the usual brain processes that allow for forgetting aren’t functioning properly, it could be beneficial to induce forgetting.
Generally, forgetting is thought of as “bad”, with people worrying about forgetting where they put the car keys, or when their wedding anniversary is. But far from being a problem, this is how memory is supposed to work. Sometimes, we want to just forget information that isn’t relevant to our daily lives, to prevent it from interfering with our goals. And sometimes, we want to forget embarrassing or emotionally scarring events.
Ultimately, the purpose of a functioning memory system is to make sensible and accurate decisions in the present, based on our past experience. The “adaptive” nature of forgetting allows us to get rid of irrelevant memories, making sure the memories that remain are as relevant to future decisions as possible. From this perspective, forgetting is as important as remembering. Simply put, forgetting is a feature of memory, not a bug.
While forgetting is a catch-all term we use for the loss of a memory, it isn’t a single process in the brain. Memories can be forgotten via active processes, such as memory suppression. But this can also happen via passive processes including “decay”, where the physical trace of a memory in the brain breaks down over time, or “interference”, where new memories that are similar to previous ones lead to confusion-impaired retrieval. For example, if you park your car in a new location in the supermarket you often visit, you might forget this new location because the usual place you park comes more readily to mind.
Forgetting is a complex phenomenon that unfolds over different timescales and via different processes, both while awake and asleep. While some memories can fragment, others are forgotten as a whole, so that all aspects of the memory are no longer accessible.
That forgetting is likely to occur during sleep has been underappreciated by psychologists, because research on sleep has largely focused on the role it plays in strengthening memories. But we and other researchers have recently reasoned that if forgetting is a fundamental part of a functioning memory system, then sleep should play as much of a role in forgetting as it does in retention.

APIMerah/Shutterstock
Previous research, including our own, has shown that the presentation of specific sounds during sleep can boost memory. If you were to learn the location of a cat on a computer screen, and during learning we played a “meow” sound, the presentation of the same sound during sleep would lead to better location memory following sleep. This selective boosting of a specific memory during sleep is called “targeted memory reactivation”.
We have recently shown that this technique can also be used to induce “selective forgetting”. We asked our participants to learn pairs of words or names before going to sleep. We used famous names, location and object words to allow participants to create vivid images in their minds for each pair, so they would be more likely to remember them after a night’s sleep.
But we also made sure the pairs overlapped by sharing one common word. When people learn these overlapping pairs, they compete against each other, and this competition can lead to forgetting some of the words. We thought a similar forgetting effect might be seen by using targeted memory reactivation when participants were sleeping.
Read more:
Why forgetting is a normal function of memory – and when to worry
We found the presentation of the word during sleep caused reactivation and strengthening for one pair, but this had a disruptive effect for the other pair. This suggests we could use targeted memory reactivation to selectively strengthen and weaken memories during sleep, presuming we can create interference between two memories. This could be beneficial in the case of people whose brain processes aren’t functioning properly, not allowing them to “healthily forget” disturbing and intrusive memories.
Although such a treatment is still a long way off, our work raises the possibility of using sound cues during sleep – in combination with psychological techniques such as cognitive behavioural therapy – to decrease the crippling emotional grip a particular memory has on a patient.
Modifying REM sleep to improve mental health
Given the strong link between REM sleep and mental health disorders, REM sleep may represent a powerful therapeutic target for treating and preventing various psychiatric conditions. By delivering sounds in synchrony with naturally occurring brain rhythms, it is possible to modify patterns of brain activity that are associated with memory processing in REM sleep.
In one study, we used a computerised algorithm to track rapidly emerging patterns of brain activity in real time while people were asleep (based on polysomnography data). When the algorithm detects the emergence of a particular brain rhythm, it delivers short bursts of sound to increase the intensity of that brain rhythm (akin to pushing a swing as it reaches the highest point of its cycle).
We have showed this technique can be used to modify distinct brain rhythms in REM sleep. In future, such auditory stimulation could potentially provide a means of renormalising aberrant patterns of brain activity in REM sleep to treat psychiatric disturbance. For example, by integrating this technology with devices that are already available for people to monitor their sleep at home, the playing of particular sounds while someone is sleeping could provide a simple and cost-effective therapy for reducing mood disturbance.
However, this is a long way from being a reality, and many studies would be required to evaluate the feasibility of such an approach before it could be used as a therapeutic tool.
Targeting sleep in psychiatric hospitals
High-risk patients undergo routine observations, sometimes as regularly as every ten minutes, all night and every night. Torches are shone into their rooms – to check they’re breathing – and there’s a lot of noise as doors are open and closed. It has a terrible impact on their sleep.
Heather* is a consultant forensic psychiatrist who works on a secure mental health ward in the North of England. She describes how the ward regime (in this case, routine welfare checks on high-risk individuals performed throughout the night) impact on patients’ sleep.
A number of people with severe mental illness receive treatment in secure inpatient units. Although the goal of these psychiatric hospitals is to provide a therapeutic setting to support the improvement of mental health, many features of the inpatient environment, such as noise at night or the ward regime, can worsen patients’ sleep disturbances – intensifying the symptoms of their illness, including low mood, impulsivity and aggression.
At the same time, chronic sleeplessness often reduces patients’ engagement with psychological therapies (due to them sleeping in the day or lacking motivation), lengthening their admission and recovery time.

APIMerah/Shutterstock
In a recent international scoping review, we found that only a small number of non-pharmacological sleep interventions had been tested in psychiatric inpatient settings, despite clear evidence that these improve both sleep and mental health outcomes.
New digital technologies can give a clear indication of patient welfare without the need for the noise and disruption Heather describes, providing an environment that is more conducive to healthy sleep. Future studies could test the potential for integrating these digital technologies with sleep-based therapies to speed up recovery times.
Achieving this goal is not only contingent on more research, but also on the capacity for carrying out scientific studies at scale. For example, all of the studies we have described were performed in tightly controlled laboratory environments, usually involving large and expensive pieces of equipment (for example, polysomnography systems). Though recent efforts have shown promise in the feasibility of moving these techniques into people’s homes, much more work needs to be done outside of the lab before digitised, sleep-focused interventions for mental illness become a reality.
We envisage a future in which sleep is a routine target for reducing or preventing symptoms of mental illness, both in psychiatric inpatient settings and in people’s homes. Although there is much work still to do, sleep research is at an exciting juncture between bench and bedside, and offers a viable solution to the growing global burden of mental illness.
*Some names in this article have been changed to protect the anonymity of the interviewees.

For you: more from our Insights series:
To hear about new Insights articles, join the hundreds of thousands of people who value The Conversation’s evidence-based news. Subscribe to our newsletter.
![]()
Scott Cairney has received funding from the Medical Research Council
Aidan Horner receives funding from the Economic and Social Research Council and the Leverhulme Trust.



























