A drug that can treat severe sickle cell disease has recently been given approval by the National Institute for Health and Care Excellence (Nice). Up to 4,000 patients in England living with sickle cell disease will now be offered voxelotor (also known under the brand name Oxbryta) to alleviate their symptoms.
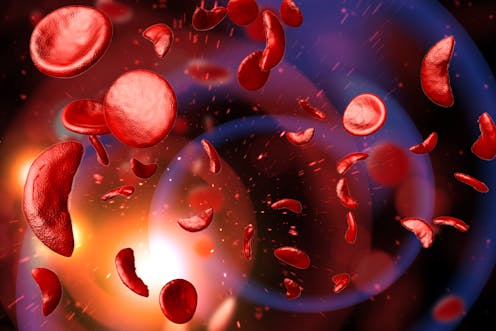
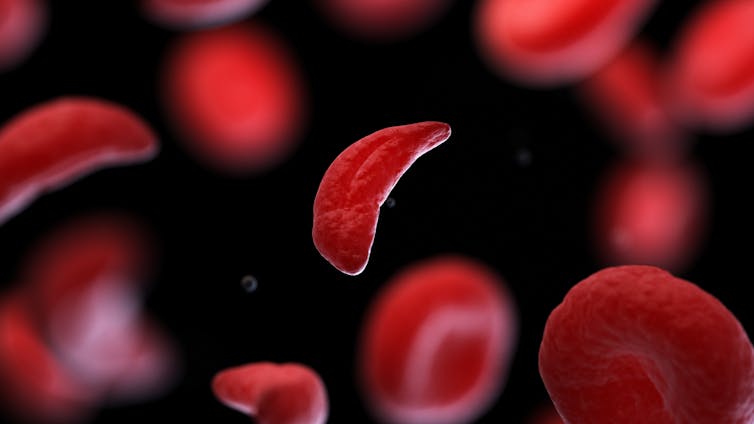
Sickle cell disease is a genetic condition that affects red blood cells, causing them to deform into a sickle shape. This can block blood flow, leading to painful episodes and severe health issues. Between 12,500 and 15,000 people in England have sickle cell disease. The disease occurs predominantly in people of African or African-Caribbean descent.
Sickle cell disease is caused by a faulty beta-globin gene. This gene provides one of the building blocks of haemoglobin – the protein inside red blood cells that bind and carry oxygen from the lungs to other tissues. In people with sickle cell disease, their haemoglobin, when not bound to oxygen, clumps together inside the cells, causing the red blood cells to become stiff and deformed.
The reason this genetic variant is relatively common among people of black African, Middle Eastern and south Asian heritage is because the altered shape of the red blood cells is inhospitable to the parasite that causes malaria. So, while this adaptation protects people from malaria, the sickle-shaped cells break down easily as a consequence. This causes a condition called haemolytic anaemia, which results in blocked blood vessels, fatigue, pain, organ damage and even death.
Voxelotor treats the root cause
For people with sickle cell disease, treatment options have mainly been limited to the drug hydroxyurea (also called hydroxycarbamide) and blood transfusions.
Hydroxyurea works by inducing the production of a foetal version of the haemoglobin gene, which allows the red blood cells to form normally. Hydroxyurea is a cheap drug that, in many patients, effectively reduces complications of sickle cell disease, such as blocked blood vessels. But the drug also lowers white blood cell count, which can weaken the immune system – making people more susceptible to infections.
Blood transfusions offer quick relief, improving oxygen levels and reducing stroke risk. However, they can cause iron buildup in vital organs such as the heart, liver and pancreas, potentially causing damage and impairing their normal functions. Immune reactions can also occur – such as transfusion-related acute lung injuries, which can be life-threatening.
Voxelotor treats the root cause of sickle cell disease by preventing the sickle-shaped haemoglobin from clumping together.
Sebastian Kaulitzki/ Shutterstock
Since sickling occurs when there isn’t enough oxygen in the bloodstream, the researchers searched for a molecule that could allow oxygen to bind to haemoglobin even when levels are low. The research led to the development of voxelotor, which corrects the root cause of sickle cell disease by increasing haemoglobin’s bond to oxygen.
The new drug can be taken alongside hydroxyurea, or on its own. Clinical trials have shown that over half of patients on voxelotor experienced a significant increase in their haemoglobin levels.
Patients have testified to the life-changing effects of the drug, noting increased energy, less fatigue, and a significant reduction in pain.
When voxelotor was first developed, there were concerns regarding the risks of a drug that alters the red blood cells’ oxygen-binding capacity while also making the blood thicker. But the first clinical trials demonstrated that it was reasonably safe when taken in the short term, with some patients only experiencing mild side-effects such as headaches or diarrhoea. But the long-term safety of this class of drug is still unknown, so will need to be answered in future clinical trials.
While voxelotor’s approval is an exciting medical advancement, one question that remains is its affordability – especially for people living in lower-income countries. The list price of voxelotor is £5,918 (excluding VAT) for a 90-pack of tablets, which lasts one month.
Pfizer, the manufacturer, has agreed on terms to provide the drug to the NHS at a discount – and Nice has specified that voxelotor will be covered by immediate funding from NHS England’s Innovative Medicines Fund. However, the challenge remains to make such treatments available and affordable worldwide.
![]()
Johan Flygare does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.



























