
Brushing your teeth is essential for maintaining optimal oral health, but like most aspects of health, the full story is more complicated.
As directors of the Center for Oral Health Research in Appalachia, we know firsthand that inequalities exist when it comes to oral health, including in children. Some people or groups have considerably more oral health problems than others because of a combination of factors beyond personal dental hygiene.
For example, Appalachia – which stretches from the northern part of Mississippi, Alabama and Georgia up through the southern part of New York, and includes all of West Virginia – has one of the greatest burdens of oral health problems per person in the U.S.
October is National Dental Hygiene Month, which provides an opportunity to draw more attention to this chronic but often preventable problem.
Table of Contents
Oral health defined
While the terms dental hygiene and dental health are largely focused on the teeth and gums, oral health is more comprehensive. According to the FDI World Dental Federation, oral health encompasses the proper functioning of the mouth, including one’s “ability to speak, smile, smell, taste, touch, chew, swallow and convey a range of emotions through facial expressions” without pain or discomfort. Oral health affects not only a person’s teeth but also overall well-being and quality of life.
Tooth decay affects children all across the U.S., but far too little attention is paid to how preventable and treatable it is. Cavities, or caries, are the most common chronic disease in kids – five times more common than asthma and seven times more common than environmental allergies, despite being preventable. More than 40% of children have tooth decay when they start kindergarten.
However, people who have less formal education or lower incomes, marginalized ethnic and racial groups and those living in more rural areas, such as Appalachia, tend to have more oral health problems than others, and at younger ages. The greater prevalence of childhood tooth decay in specific populations is not only an inequity but also a serious public health problem. Oral health problems early in life extend into adulthood and can be lifelong.
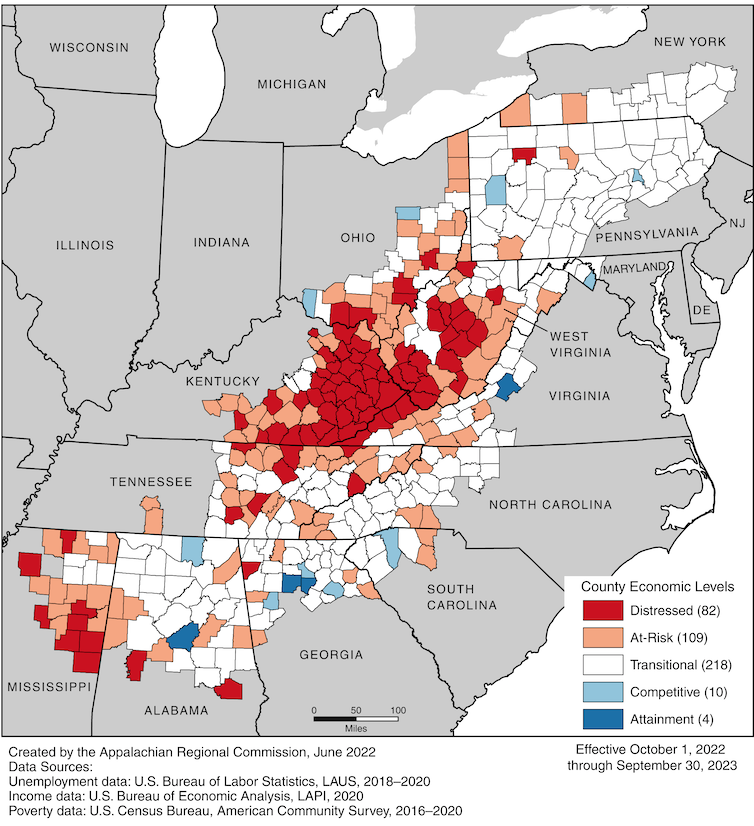
Appalachian Regional Commission
Beyond personal dental hygiene
It’s a common misconception that consuming sugary foods and beverages is the only cause of tooth decay. While that is undoubtedly a problem, there’s much more to good oral health. It includes consistent brushing and flossing; eating healthy foods, like fresh fruits and vegetables; avoiding tobacco products; and wearing mouth guards while playing certain sports. Regular visits for dental care are also critical, as they provide an opportunity for cleanings and preventive care.
Oral health in kids is a reflection of their overall health and that of their families; however, in addition to behavioral and social influences, genetic and other biological factors are also at play. For example, genes influencing taste preferences – such as those for sweet foods – are associated with cavities on certain teeth and surfaces of teeth. It’s possible that our taste genes predispose some of us to prefer consuming sweet foods and drinks, which is a risk factor for developing cavities.
Bacteria and other microorganisms in the mouth, known as the oral microbiome, also play a role. Some parts of the oral microbiome are beneficial and even required for good oral health. Other bacteria are invaders that can lead to oral diseases.
Just as important are environmental factors, including air quality, access to healthy foods, the cost of dental care, access to transportation to and from the dentist, and school-based programs that encourage good oral hygiene among children. Whether one lives in a community with fluoridated water or otherwise has access to fluoride treatments is also important, as fluoride helps to prevent tooth decay. Water quality in communities is another factor. If the only available water is toxic or unappealing, people may turn to soda and other sugar-sweetened beverages.
Additionally, mothers’ perceived social support and parents’ social networks can influence their children’s oral health too. Among mothers with a high number of cavities, the availability of someone to talk to about problems has been shown to be associated with fewer cavities in their children.

Nitat Termmee/Moment via Getty Images
Role modeling good oral health
Parents’ and caregivers’ own oral health greatly influences that of their children. Kids and their parents typically drink the same water and many of the same beverages and eat a lot of the same foods. Children often follow the dental hygiene habits of their parents as well. Children typically take on their parents’ and caregivers’ feelings about dental visits too – whether it’s comfort, stress, anxiety or fear.
Parents’ thoughts about dental care influence their decisions about preventive care. Dental fear and anxiety can lead to delay or avoidance of dental appointments for themselves and their children. “Oral health values” – the importance one places on maintaining natural and good-looking teeth – affect decision-making about dental hygiene and professional dental care. Depression in parents can even influence their own dental hygiene and oral health and that of their children.
Dental problems in kids can lead to missed school, pain and embarrassment about visible decay, and missing or crooked teeth. Teeth and gums are critical for speaking, eating, development and appearance. They affect social functioning and one’s enjoyment of food. Kids’ dental problems affect their parents, too, as they can result in parents’ unexpectedly missing work to bring their child to the dentist.
What can be done to improve oral health?
To a great extent, dental problems in kids can be prevented. Some preventive steps are affected by economic, educational and health care factors. One of the best things parents or caregivers can do is to establish a relationship for their child with a dental practitioner, practice, office or clinic to promote prevention but also to provide emergency care if needed. Within the oral health world, this relationship is called a “dental home.” The American Academy of Pediatric Dentistry and other professional health organizations recommend that children see an oral health care provider before age 1 or at the emergence of the first tooth. Access to dental treatment, especially preventive care, has been shown to improve oral health in families and their communities.
System-level changes are surely needed too. Since cost affects whether parents can provide their children with routine dental care, greater access to dental insurance is an important step to ensuring equal access and reducing oral health inequities. Integrating oral health practices into schools and educational programs is another system-level change that would benefit all children regardless of their family’s socioeconomic status.
Oral health is a critical factor in a person’s overall health. Teaching kids this early can help them develop a healthy smile and care for their pearly whites throughout their lives.
![]()
Daniel W. McNeil receives funding from the National Institutes of Health, including the National Institute of Dental and Craniofacial Research.
Mary L. Marazita receives funding from the National Institutions of Health, specifically the National Institute of Dental and Craniofacial Research (NIDCR).























