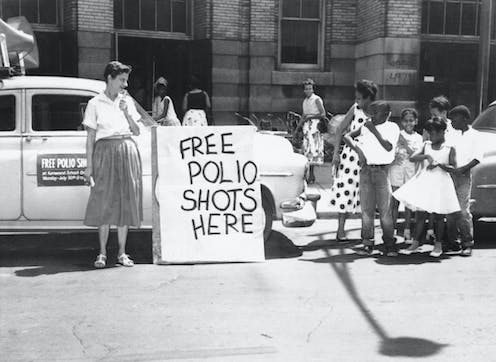
Given recent headlines, you may be wondering why polio is even an issue in 2022. For more than 60 years, vaccines against the poliovirus have protected virtually everyone in the United States from the disease. Due to an enormously successful polio vaccination campaign beginning in the 1950s when the first polio vaccines became available, by 1979 polio was considered eliminated in the U.S.
Unfortunately, even today, there are communities in the U.S. that have lower-than-necessary polio vaccination rates. Because many people have not been vaccinated, there is now a real possibility of a resurgence of polio in the U.S.
As a clinical professor of pharmacy, I train future pharmacists about how vaccines work, their importance and how they prevent diseases.
Public health experts’ longstanding concerns over falling vaccination rates rose to the surface when, in July 2022, a man from Rockland County, New York, was diagnosed with polio, the first such diagnosis in the U.S. in nearly a decade. The patient – who developed the severe, paralytic form of the disease – had been exposed to an altered live vaccine strain from overseas.
Then on Sept. 9, 2022, New York declared a state of emergency due to ongoing poliovirus transmission. As of that date, using wastewater surveillance, officials had identified 57 samples of poliovirus in wastewater from four New York counties. More than half of those were detected in the same county where the adult patient is from, just outside New York City.
As a result of the continued poliovirus detection in wastewater, the Centers for Disease Control and Prevention declared that the U.S. now meets the World Health Organization’s criteria for “a country with circulating vaccine-derived poliovirus.”
Table of Contents
Two main poliovirus vaccine types
There are two key types of polio vaccine in use around the world today. The inactivated poliovirus vaccine is given as a shot, and the oral attenuated (or weakened) poliovirus vaccine is administered as oral drops, sometimes on a sugar cube.
Since 2000, the U.S. has exclusively used the inactivated poliovirus vaccine, which cannot cause disease since it does not contain live virus. But in countries where the poliovirus continues to circulate, such as Pakistan and Afghanistan, the oral attenuated poliovirus vaccine is still used.
In extremely rare cases, the weakened live vaccine used in other countries can mutate back into its virulent form and lead to paralysis. This is how the adult in New York is believed to have come into contact with the virus.
How ‘herd immunity’ for polio is determined
The degree to which a community is protected from a pathogen like poliovirus comes down to herd immunity. When a community – the so-called herd – reaches a threshold of immunity, it can prevent the transmission of a pathogen from person to person, thereby quelling the pathogen.
The herd immunity threshold for a given disease is calculated based upon the expected number of individuals who an infected person would spread it to if they were susceptible. The higher the number of individuals who would become infected, the higher the percentage of the community or population that needs to be vaccinated to avoid continued spread of the disease.
For poliovirus, researchers estimate that between five and seven individuals would be infected for each case if those people were susceptible. Based upon these calculations, experts determined that at least 80% of a community or population should be vaccinated against poliovirus to prevent its spread.
Falling vaccination rates
Throughout the U.S., vaccination rates for polio vary significantly.
The CDC recommends that infants and young children receive a four-dose schedule of the inactivated poliovirus vaccine at 2 months, 4 months, 6 to 18 months and 4 to 6 years. For those who begin vaccination later – as older children, teens or adults – three doses is considered to be complete vaccination. This is because three doses of inactivated poliovirus vaccination have been shown to provide between 99% and 100% protection against severe disease.
Although all U.S. states are currently above the 80% herd immunity threshold for poliovirus, there are areas within the country that include many pockets of unvaccinated or undervaccinated individuals – those who have not received a total of three lifetime doses of the inactivated vaccine.
New York state, for example, holds one of the highest kindergarten polio vaccination rates in the country, with 97.9% of kindergartners vaccinated in the 2020-2021 school year. But current estimates by the New York State Department of Public Health suggest that only 79% of 2-year-olds in that state have received three doses of the polio vaccine.
Further, in certain pockets and counties of New York, such as Rockland, Orange and Sullivan, three-dose vaccination rates may be far lower based on the 2-year-old age group, which is the only data that is available by county: Rockland 60%, Orange 59% and Sullivan 62%. In fact, 46% of counties in New York are below the three-dose poliovirus vaccination herd immunity threshold for 2-years-olds.
Vaccine recommendations
When children fall more than one month behind on recommended polio vaccination, doctors recommend routine catch-up throughout adolescence.
Because most adults in the U.S. today were vaccinated as children and the U.S. had eliminated polio as of 1979, there was little reason for health experts to believe an adult would come into contact with poliovirus in the U.S. For that reason, catch-up vaccination for adults has not been included on the routine adult vaccination schedule.
But in August 2022, the CDC updated its guidelines. In light of the fact that there are communities where poliovirus vaccination rates have fallen below the 80% threshold needed for herd immunity, coupled with the ongoing circulation of poliovirus in New York, the CDC now recommends that all unvaccinated or undervaccinated adults receive a poliovirus vaccination.
Additionally, the CDC suggests that some fully vaccinated adults who are at increased risk of exposure may benefit from a single lifetime poliovirus booster dose. This includes health care providers who care for those with poliovirus, or people traveling to areas where poliovirus has not been eliminated.
If you are unsure if you need vaccination or what steps you should take, talk to your pharmacist or primary care physician.
![]()
Jennifer Girotto consults for Lexi-Comp. She has received grant funds from Pfizer to support independent quality improvement specific to outpatient antimicrobial stewardship.
























