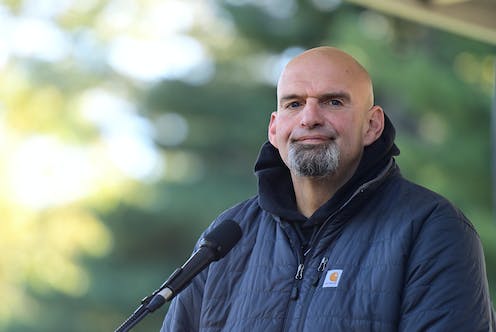
John Fetterman, the Democratic nominee for a hotly contested U.S. Senate seat in Pennsylvania, has been drawing scrutiny for his performance in his first post-stroke broadcast interview and most recently, his Oct. 25, 2022, Senate debate against Republican Mehmet Oz.
Fetterman suffered a stroke on the way to a campaign event in May 2022. His apparent post-stroke neurological effects – including auditory processing and speech issues – have caused some to question his fitness for the role and have become a central factor in the Senate race. The Conversation asked Andrew Southerland, a vascular neurologist specializing in stroke and cerebrovascular disease who sees many patients like Fetterman, to explain what Fetterman’s case can teach us about stroke recovery.
Table of Contents
What does the public know about Fetterman’s stroke?
Fetterman has chosen not to release his full medical record, so it’s not possible to draw conclusions about the exact location or extent of brain injury resulting from his stroke. He and his team have confirmed that his initial symptoms began with feeling fatigued and slurring his speech, which his wife immediately identified as a possible stroke.
Because of her early recognition of his symptoms and rapid transport to a nearby facility, Lancaster General Hospital in Pennsylvania, he had the opportunity to receive a clot-busting drug called a thrombolytic and underwent a catheter-based procedure to remove the blood clot from an artery in the brain.
Based on this information, experts know that Fetterman suffered an ischemic stroke caused by a blockage of blood flow and oxygen to a certain part of the brain. Ischemic stroke accounts for roughly 85% of the 800,000 new cases of stroke occurring each year in the United States. The remainder are hemorrhagic strokes caused by bleeding in or around the brain.
Ischemic stroke often results in a collage of symptoms including facial droop, speech changes and limb weakness, numbness or lack of coordination on one side of the body. These symptoms help bystanders recognize the signs of stroke. When treating ischemic stroke, we in the stroke community use the motto, “Time Is Brain,” because the sooner we can restore blood flow to the brain after a stroke begins the better chance the patient has of making a good recovery.
Fetterman has said publicly that his stroke occurred due to an abnormal rhythm of the heart called atrial fibrillation. This is a common cause of ischemic stroke, which happens when blood clots form in the heart and travel – or embolize – to the brain. This is the origin of the term “thromboembolism,” which basically means blood clot traveling from one location to another. In the case of atrial fibrillation causing stroke, it refers to a blood clot traveling through arteries from the heart into the brain.
Fortunately, these types of stroke are highly preventable simply by taking a daily anticoagulant to prevent the clots from forming. Atrial fibrillation may cause symptoms of fast heart beat or shortness of breath. But often, it is silent, coming and going in short episodes. This makes it more challenging to diagnose and treat. Current guidelines recommend starting an anticoagulant for stroke prevention in high-risk patients with atrial fibrillation.
Why can stroke lead to auditory processing issues?
Just like any organ or tissue in the body, normal function in the brain depends on steady blood flow and oxygen. Interruptions in this blood flow – as is the case in ischemic stroke – can lead to permanent injury called infarction. The location and extent of infarction after a stroke determine what deficits a patient suffer.
In the case of an auditory processing issue, the injury occurs in a part of the brain called the temporal lobe affecting the connection between areas where auditory and language processing occur. In other words, a stroke can disrupt how we hear and process words.
Recovery from stroke depends on a number of variables, including a patient’s age and other medical problems, but largely on the extent of the injury and where it occurs in the brain.
How do auditory processing issues relate to cognition?
Auditory processing disorders fall under a larger family of stroke deficits termed aphasia, which have to do with one’s ability to produce or comprehend various forms of language. Aphasia is often categorized as expressive, related to difficulty producing language, or receptive, meaning a difficulty understanding language.
The types of things that aphasia can affect include word finding, grammar, naming, reading and writing. Patients with aphasia can also struggle with paraphasic errors – in other words, saying an incorrect word that sounds like the intended word they are trying to say.
Fetterman identified this specific challenge during his NBC News interview, pointing to the example of his saying “emphetic” in place of the word “empathetic.” These issues often get worse during high-pressure situations like debates. What’s unique in Fetterman’s situation is that reading words seems to be easier than hearing them, hence the use of closed captioning during his NBC News interview and his debate.
Aphasia is a common symptom of stroke but can also occur in other neurological conditions including various types of dementia.
Most importantly, aphasias and auditory processing disorders do not necessarily imply other cognitive impairments. In other words, they typically do not alter one’s intelligence, behaviors or executive abilities – neurological functions that are orchestrated by the frontal lobes of the brain.
What is the typical path of recovery following stroke?
Fetterman now joins the ranks of more than 7 million Americans and many more around the world who have suffered a stroke, a significant portion of whom remain disabled as a result. Yet, advances in life saving treatments – like the ones Fetterman received – provide hope for stroke patients who were once destined for permanent disability to now walk out of the hospital and return to independent, high-functioning lives.
Typically, recovery from stroke occurs along a continuum, from the early hospitalization to a prolonged period of rehabilitation over weeks to months. Depending on the severity of the stroke and resulting deficits, this may require a period of time in an inpatient rehabilitation facility and possibly working with physical, occupational and speech therapists in an outpatient setting. In either case, stroke rehabilitation and recovery is a team sport, requiring collaboration from a multi-disciplinary group of providers along with the support of patient caregivers.
In the field of stroke recovery, patients gain the most ground in the first few months following a stroke event. However, recovery experts know that patients can continue to see gradual improvements well into the first year and beyond.
One thing that’s certain is that stroke survivors like Fetterman are a testament to the advances in clinical research and practice that paved the way for the life-saving treatments like the ones he received. And there’s nothing debatable about that.
![]()
Andrew M. Southerland, MD, MSc receives funding from the NIH/NINDS, American Heart Association/American Stroke Association, Abbvie, Inc, and Diffusion Pharmaceuticals, Inc. He is affiliated with the American Academy of Neurology’s BrainPAC Executive Committee.





























